In a dramatic testimony before the Senate Finance Committee last Thursday, Health and Human Services Secretary Robert F. Kennedy Jr. declared again that the United States is “the sickest country in the world.”
He attributed this status to chronic diseases, lack of physical activity, and failures within the Centers for Disease Control and Prevention (CDC).
- RFK Jr. called the U.S. the "sickest country in the world," citing chronic diseases, inactivity, and CDC failures during a Senate hearing.
- The U.S. ranks last among 10 other high-income countries in health system performance and struggles with life expectancy and preventable deaths.
- Obesity affects 42% of Americans, 134% higher than peer countries, costing $173 billion annually and linked to diet and inactivity issues.
- Political conflicts on vaccine policies and CDC leadership have politicized public health, risking trust and children's health in the U.S.
“If we don’t end this chronic disease, we are the sickest country in the world,” he said. “That’s why we have to fire people at CDC. They did not do their job. This was their job to keep us healthy.”
But how accurate are RFK Jr.’s claims? A closer look at the data and studies on U.S. health-care access and lifestyle factors shows a complex picture.
RFK Jr. called the U.S. ‘the sickest country in the world’ at a Senate hearing last week
Image credits: Andrew Harnik/Getty Images
In late August, the Trump administration fired Susan Monarez, the then-director of the CDC. The move triggered resignations from other top officials at the center.
RFK Jr. argued that firing certain CDC officials was necessary to fix what he described as a broken public health system.
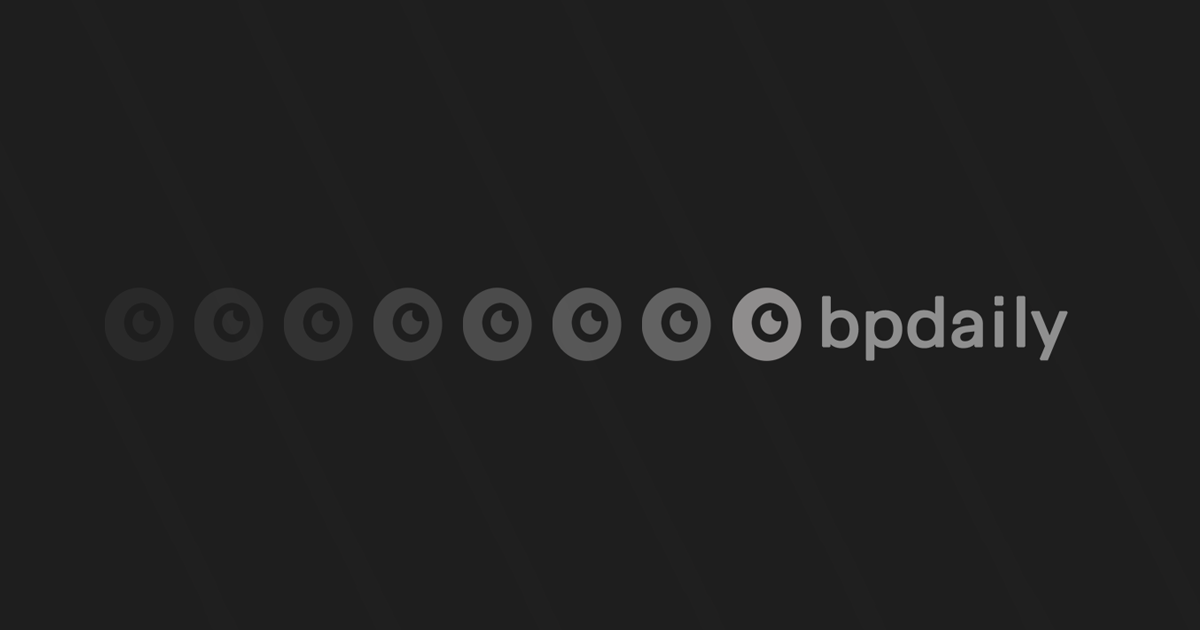
The U.S. spends more on health care than any other country. Yet, a 2024 Commonwealth Fund report ranks the U.S. last on health system performance among 10 other high-income countries, including Australia, Canada, France, Germany, the Netherlands, New Zealand, Sweden, Switzerland, and the U.K.
The report examined five key areas: access to care, care process, administrative efficiency, equity, and health outcomes.
Image credits: Commonwealth Fund
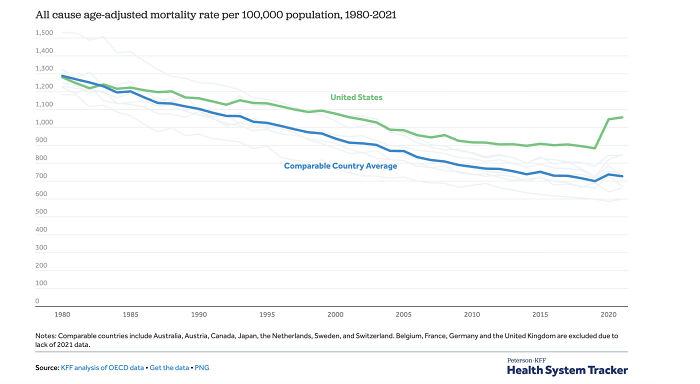
The U.S. struggles particularly with health outcomes. Life expectancy lags more than four years behind the average of peer countries, and it has the highest percentage of preventable and treatable deaths, including excess deaths during the COVID-19 pandemic, for people under 75.
Social issues, such as substance abuse, with over 100,000 overdose deaths in 2023, also contributed to poor health outcomes.
The country’s fragmented insurance system leaves 26 million Americans uninsured, leading to about 40% of adults reporting delaying or skipping care due to the fear of costs.
One of RFK Jr.’s main targets is lifestyle, particularly diet and physical activity. A studycomparing the U.S. to Spain, Italy, Iceland, Japan, and Switzerland found American obesity rates were 134% higher than the average of the five countries, standing at 42%.
Image credits: Michael Siluk/Getty Images
The CDC estimates obesity costs the U.S. healthcare system $173 billion each year.
Dietary patterns in the U.S. also raise concerns. American cuisine tends to be more heavily processed, with larger portion sizes and consisting of 10% more sugar in meals when compared to the five countries in the study.
Such diets have been linked to increased risks of obesity, Type 2 diabetes, and some types of cancers.
Meals are often eaten on the go, coupled with physical inactivity, both leading to higher obesity rates, which are linked to cardiovascular disorders.
While self-reported exercise in the U.S. is similar to other countries, American dependence on cars is 35% higher than in peer countries, which reduces incidental physical activity.
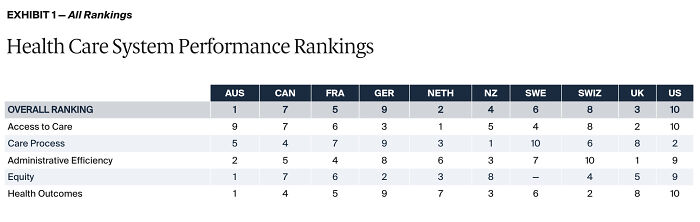
About a third of U.S. adults live with multiple chronic conditions, the highest proportion among high-income nations. Hypertension, chronic obstructive pulmonary disease, and diabetes are particularly common.
Dietary patterns, chronic diseases, and physical inactivity raise health concerns in the U.S.
Image credits: The Wall Street Journal
These chronic diseases are one of the biggest drivers of early deaths in the U.S.
Many of these are preventable and linked to smoking, alcohol use, physical inactivity, and poor nutrition.
A study published in JAMA Health Forum indicates that in 2022 and 2023, over 1.5 million deaths in the U.S. could have been prevented if mortality rates matched those of peer high-income countries.
This “missing Americans” trend has been on the increase for decades, particularly among working-age adults.
“The US has been in a protracted health crisis for decades, with health outcomes far worse than other high-income countries,” Jacob Bor, associate professor of global health and epidemiology at Boston University, told BU School of Public Health.
“Americans die earlier and are sicker than people in other high-income countries,” Dr. Steven Woolf, a life-expectancy researcher at the Virginia Commonwealth University, told The Wall Street Journal. “This has been true for a long time, and the trend is getting worse.”
Image credits: Peterson-KFF Health System Tracker
In addition, public health experts also point to stress and socio-economic inequality as critical factors affecting U.S. health.
The American Psychological Association’s Stress in America survey reports that about 75% of U.S. adults say they’ve experienced physical or emotional symptoms of stress in the past month.
Gallup’s 2023 Global Emotions Report reveals that nearly half of Americans—about 49%—deal with significant daily stress, ranking the U.S. among the most stressed high-income countries.
RFK Jr.’s claim that Americans are “chronically sick” has some grounding in these statistics. The U.S. consistently ranks last among wealthy nations in several health metrics, such as life expectancy, infant and maternal mortality, and avoidable deaths — despite massive investment in health care.
While we can assert that the U.S. stands out for its poor health results among wealthier countries, to call it the “sickest country in the world” is misleading if noting that many lower-income countries have worse outcomes.
Researchers have also blamed the fractured U.S. health system as a contributor to the lagging health.
Yet, the proposals and exaggerated statistics put forward by Republican senators do not offer a clear path to improving U.S. health. For instance, Republican Sen. Roger Marshall suggested children receive “too many” vaccines, citing numbers like 76 shots.
The U.S. ranks the lowest on health indicators compared to other high-income countries
Image credits: Joe Raedle/Getty Images
In reality, children typically receive about 30 doses by age 2, many of which are combined in single shots. The CDC itself states that this does not overwhelm the immune system.
RFK Jr. also claims that there was no clinical data to support COVID-19 vaccines, and Sen. Ron Johnson said there are thousands of deaths linked to COVID-19 vaccines.
A fact check by ABC News revealed both of these statements to be untrue, setting a dangerous precedent for the health system.
The hearing became particularly explosive when Democratic Senators Elizabeth Warren and Bernie Sanders pressed RFK Jr.
Warren accused him of lying about his vaccine policies, arguing that RFK Jr.’s decision not to recommend the vaccine effectively removes access to the shot.
Sanders challenged RFK Jr. on his claim that U.S. public health agencies are influenced by pharmaceutical interests, arguing that industry ties with big pharma undermine both science and trust in health guidance.
He noted that nearly every Republican senator and many Democrats received Political Action Committee (PAC) donations from the drug industry, but said RFK Jr. believed that everybody but him was corrupt.
While the FDA’s funding is made up of federal government budget allocation, a huge chunk of its finances includes fees paid by industries regulated by the FDA, including pharmaceutical companies.
Critics argue that these financial arrangements create at least a perceived conflict of interest, raising questions about whether regulatory decisions fully prioritize public health. Yet the available evidence shows that, despite these concerns, COVID-19 vaccines have had a huge impact.
A study published in PubMed Central estimated that COVID-19 vaccines prevented approximately 14.4 million deaths worldwide, and another study cited that 3 million lives were saved in the U.S.
Democratic Sen. Michael Bennet argued during the hearing that RFK Jr. has “elevated conspiracy theorists” and “crackpots” during his tenure as secretary, with his priority being to take vaccines away from Americans.
Democratic Sen. Ron Wyden added, “Robert RFK Jr. puts children in harm’s way every single day in America.”
These statements echo those of the top officials who left the CDC after Monarez was fired, warning the American public about the politicization of the Department of Health.
Image credits: Andrew Harnik/Getty Images
“Their desire to please a political base will result in death and disability of vulnerable children and adults,” Dr. Demetre Daskalakis, director of the National Center for Immunization and Respiratory Diseases, wrote in his resignation letter.
“Their base should be the people they serve, not a political voting bloc,” he added.
He accused people of “dubious scientific rigor” being put in charge of the COVID-19 vaccine workgroup.
Despite the political wrangling, the outlook for Americans’ health remains bleak.
Comparisons with countries like Italy, Spain, Japan, and the U.K. illustrate where the U.S. could improve. Mediterranean diets are rich in unprocessed foods, fruit, vegetables, and fish, and can contribute to lower obesity and chronic disease rates.
Active transportation, shorter work hours, and most importantly, a health-care system designed to foster a healthier population all contribute to overall wellness.
Poll Question
Thanks! Check out the results:
If he means morally sick with the Trump regime's psychopathy, I would agree 100%.
If he means morally sick with the Trump regime's psychopathy, I would agree 100%.







14
1